Despite having medical transportation insurance, millions of Americans depend on ambulance services annually, and many of them incur unforeseen medical expenses.
Knowing your options for filing an ambulance reimbursement insurance claim can greatly reduce the financial strain that emergency medical services can cause.
Although navigating the claim filing process can be difficult, it’s an essential step in getting the coverage to which you are legally entitled. This post will explain what your insurance covers and give you a detailed, easy-to-follow guide on how to submit a successful claim.
Understanding Ambulance Insurance Coverage
To make sure you’re sufficiently covered in medical emergencies, it’s critical to comprehend the specifics of ambulance insurance. Emergency or non-emergency ambulance services can be expensive, and your financial burden can be greatly reduced by understanding what your insurance will cover.
Emergency vs. Non-Emergency Transport Coverage
Emergency and non-emergency transports are frequently distinguished in insurance coverage for ambulance services. Since emergency transports are deemed medically necessary, they are usually covered by most insurance plans. However, depending on the insurance company and the particular policy, non-emergency transports, like planned medical visits, might have different levels of coverage.
Medicare Part B, for example, may not cover non-emergency ambulance services unless certain requirements are met, but it does cover emergency ambulance services when they are considered medically necessary.
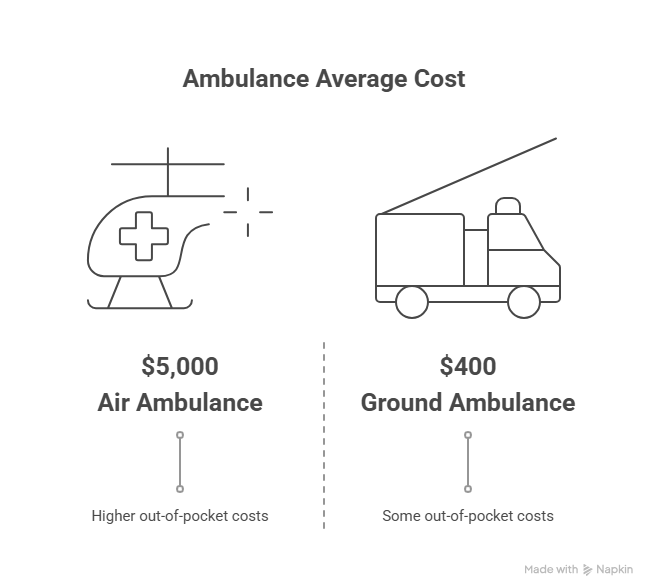
Ground vs. Air Ambulance Reimbursement
Insurance coverage may also be impacted by the kind of ambulance service utilized. Compared to air ambulance services, ground ambulance services are typically more prevalent and have different reimbursement rates. Despite being more costly, air ambulance services are frequently required for long-distance transports or in circumstances where ground transport is impractical.
| Service Type | Typical Coverage | Average Cost |
|---|---|---|
| Ground Ambulance | Generally covered, with some out-of-pocket costs | $400-$1,000 |
| Air Ambulance | Often requires pre-approval; higher out-of-pocket costs | $5,000-$20,000+ |
Medicare, Medicaid, and Private Insurance Differences
The coverage of ambulance services is subject to change depending on the insurance company. For ambulance services to be covered by Medicare and Medicaid, certain requirements must be met. Although private insurance companies can differ greatly from one another, they might provide more extensive coverage.
For instance, while some private insurance plans might require extra riders for non-emergency transports, others might cover both emergency and non-emergency ambulance services.
Filing an Ambulance Reimbursement Insurance Claim
Taking a methodical approach can help you navigate the intricacies of ambulance reimbursement claims. Careful planning, close attention to detail, and process knowledge are necessary when filing a claim.
Essential Documentation and Paperwork
You will need to collect certain documents in order to submit an ambulance reimbursement insurance claim. Usually, these consist of:
- The report from the ambulance service
- Records of medical care associated with the transport
- Form for filing an insurance claim
- Evidence of insurance
The claims procedure will go more smoothly if you have all the required documentation.
Step-by-Step Claim Submission Process
A few crucial steps must be taken in order to submit an ambulance insurance claim:
- Fill out the insurance claim form completely.
- Include all necessary documentation.
- Send the insurance company the claim.
- Check the status of the claim.
To prevent delays or denials, it is essential to adhere to the particular instructions provided by the insurance provider when submitting a claim.
Claim Filing Deadlines and Timelines
There are deadlines for submitting claims to insurance companies. Claims may be rejected if these deadlines are missed. It is imperative that:
- Recognize when the insurance company requires claims to be filed.
- Send in claims as soon as possible.
- Monitor the status of the claim.
Handling Claim Denials and Appeals
Don’t give up if a claim is rejected. The decision can be appealed by:
- Examining the reason for denial
- obtaining more data or supporting documentation
- Making a request to the insurance company
The secret to a successful appeal is perseverance and careful planning.
Conclusion
Although navigating insurance reimbursement for ambulances can be challenging, the burden can be greatly reduced by being aware of the subtleties of coverage and the claims procedure. People can better understand what their insurance plans cover by differentiating between ground and air ambulance services, as well as between emergency and non-emergency transport.
For both patients and insurance companies, efficient ambulance billing services are essential to expediting the reimbursement process. A seamless experience depends on making sure that claims are submitted accurately and within the allotted time frames.
Because insurance for ambulance providers is intended to make it easier to get paid for services rendered, it is crucial that providers comprehend the nuances of insurance coverage. They can reduce the number of claims that are denied and guarantee that patients get the money they need by doing this.
In the end, knowing the ins and outs of insurance coverage and ambulance reimbursement enables people to make well-informed choices about their medical transport requirements. A simpler route to reimbursement and less financial strain may result from this clarity.
FAQ
What is insurance for ambulance reimbursement?
In the event that you require medical attention while traveling to a medical facility, ambulance reimbursement insurance can assist in covering the cost of ambulance services, including both emergency and non-emergency transportation.
What is normally covered by insurance coverage for ambulances?
Transportation to and from medical facilities, both emergency and non-emergency, as well as transportation between facilities for specialized care, are usually covered by ambulance insurance. Depending on the insurance company and policy, coverage may change.
How can I submit a claim for insurance reimbursement for an ambulance?
You must collect the necessary paperwork, such as the ambulance service report, medical records, and insurance information, before submitting the claim to your insurance company in accordance with their particular policies in order to file an ambulance reimbursement insurance claim.
What distinguishes air ambulance reimbursement from ground ambulance reimbursement?
While air ambulance reimbursement covers air transportation, usually for more urgent or long-distance situations, ground ambulance reimbursement usually covers land transportation. The two may have different rates of coverage and reimbursement.
What are the differences in ambulance coverage between private insurance, Medicaid, and Medicare?
The reimbursement rates and coverage requirements for ambulance services vary amongst private insurance companies, Medicare, and Medicaid. Private insurance might provide more extensive coverage, but it’s important to verify your particular policy. Medicare and Medicaid, on the other hand, frequently have stricter requirements.
What occurs if my insurance claim for an ambulance is rejected?
You can challenge the decision if your ambulance insurance claim is rejected by submitting more supporting documentation. Following the insurance provider’s appeals procedure and comprehending the rationale behind the denial are essential.
Are there any deadlines for submitting an insurance claim for ambulance reimbursement?
Yes, depending on the insurance company, there are typically deadlines for submitting an ambulance reimbursement insurance claim. To find out the filing deadline, you must consult your policy or get in touch with your insurance company.
Can I get assistance with the claims process by using ambulance billing services?
In order to facilitate the reimbursement process, ambulance billing services can help with the claims process, including preparing and submitting claims, managing denials, and guaranteeing adherence to insurance regulations.
How can I make sure my insurance claim for an ambulance is handled properly?
Provide accurate and comprehensive documentation, adhere to the insurance provider’s instructions, and proofread your claim for mistakes or omissions before submitting it to guarantee your ambulance insurance claim is handled appropriately.