It can be difficult to navigate the dental insurance landscape, particularly when it comes to submitting claims. Did you know that small mistakes or omissions result in the denial of almost 25% of dental insurance claims? This startling figure emphasizes how crucial it is to comprehend how dental insurance claims are processed.
Understanding the required procedures and best practices is essential to guaranteeing a seamless reimbursement experience. You can increase your chances of approval and steer clear of common pitfalls by understanding the basics of dental treatment reimbursement.
You can successfully negotiate the intricacies of dental insurance and obtain the compensation you are entitled to with the correct advice.
Understanding Dental Insurance Coverage
It’s critical to understand your insurance plan in order to optimize your dental benefits. You can make better decisions regarding your oral health by being aware of the wide variations in dental insurance coverage.
Types of Dental Insurance Plans
PPO (Preferred Provider Organization) and DHMO (Dental Health Maintenance Organization) are two of the various kinds of dental insurance plans. While DHMO plans are frequently more affordable but restrict your options for providers, PPO plans give you greater freedom in selecting your dentist.
What Procedures Are Typically Covered
Preventive care like cleanings and exams are typically covered by dental insurance plans. Basic procedures like extractions and fillings are also covered by many plans. Coverage for more involved procedures, such as orthodontics or crowns, can differ, though.
Deductibles, Co-pays, and Annual Maximums
It’s critical to comprehend annual maximums, co-pays, and deductibles. Annual maximums are the highest sums your insurer will pay in a given year, co-pays are your portion of the expenses after you meet the deductible, and deductibles are the sums you pay before insurance takes effect.
Dental Treatment Reimbursement Steps
It can be difficult to navigate the dental treatment reimbursement process, but it can be made easier by knowing the steps. From preparing for the appointment to submitting a claim, there are a number of important steps in the process.
Before Your Dental Appointment
Verifying Your Benefits
It’s important to confirm your insurance benefits prior to your dental appointment. To find out which procedures are covered and how much they will cost, get in touch with your insurance company.
Obtaining Pre-authorization
Pre-authorization is necessary for certain treatments. To prevent any problems with your claim, make sure you get this prior to your appointment.
During Your Dental Visit
Essential Documentation to Request
Ask for a thorough explanation of the treatments you received during your visit, along with procedure codes and descriptions. You must have this paperwork in order to submit your claim.
Understanding Procedure Codes
You can handle the reimbursement process more skillfully if you are aware of the procedure codes your dentist uses.
Filing Your Claim
Completing Insurance Forms Correctly
Make sure you accurately fill out the insurance forms when submitting your claim. Any mistakes could result in denials or delays.
Submitting Supporting Documentation
Include all required supporting documentation with your claim, such as receipts and thorough treatment descriptions.
Tracking Your Claim Status
Check the status of your claim after submitting it. For this reason, the majority of insurance companies provide customer service lines or web portals.
You can guarantee a more seamless reimbursement procedure for your dental procedures by adhering to these guidelines.
Tips to Maximize Reimbursement Approval
Knowing the typical mistakes that result in claim denials is crucial if you want to increase the likelihood that your dental reimbursement will be approved. You can take precautions to prevent these possible problems and guarantee a seamless claims procedure by being aware of them.
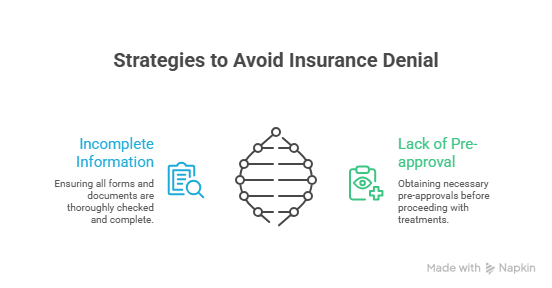
Common Reasons for Claim Denials
Claims are frequently rejected because of non-covered services, missing or erroneous information, or a lack of pre-approval. Make sure to thoroughly read your insurance policy and submit all necessary paperwork to prevent these problems.
| Reason for Denial | Prevention Strategy |
|---|---|
| Incomplete Information | Double-check all forms and documentation |
| Lack of Pre-approval | Obtain pre-approval before treatment |
| Non-covered Services | Review insurance policy to understand covered services |
Effective Appeal Strategies
Don’t give up if your claim is rejected. By offering more details or context, you can challenge the ruling. A letter from your dentist or other supporting documentation may be part of this.
Working with Your Dental Office for Support
When it comes to the reimbursement process, your dental office may be a useful resource. They can offer advice on the claims procedure and assist you in resolving any problems that may come up.
Digital Tools and Apps for Claim Management
You can handle your dental insurance claims with the aid of numerous apps and digital tools. These can assist you in maintaining organization and control over the reimbursement procedure.
Navigating Dental Treatment Reimbursement with Confidence
A seamless reimbursement process depends on knowing what your dental insurance covers. You can guarantee a hassle-free experience by being aware of the procedures required to submit a claim for reimbursement and by heeding the advice provided. You can make more informed decisions about your dental care if you are aware of the different types of dental insurance plans, covered procedures, deductibles, co-pays, and annual maximums.
You can increase the likelihood that your claim will be approved for reimbursement by following the proper procedures before, during, and after your dental visit and by using digital tools for claim management. The secret to confidently navigating the dental treatment reimbursement process is to remain proactive and informed.
FAQ
How long does it usually take for dental insurance to reimburse?
Generally speaking, dental insurance reimbursement takes anywhere from a few days to several weeks, though this varies based on the insurance company. The best course of action is to inquire about the precise processing times of your insurance provider.
Before a procedure, how can I confirm my dental benefits?
Check your insurance company’s website or get in touch with them directly to confirm your dental benefits. Additionally, you can request that your dentist’s office confirm your benefits. Usually, they will require your insurance details in order to verify your coverage.
What paperwork is needed to submit a dental insurance claim?
A filled-out claim form, a thorough explanation of the procedure, and occasionally X-rays or other diagnostic pictures are the necessary paperwork for a dental insurance claim. The required paperwork will typically be provided by your dentist’s office.
Can I file an appeal after my dental insurance claim is rejected?
A denied dental insurance claim can be appealed, yes. Examining the letter of denial and comprehending the rationale behind it is the first step. After that, collect any further data or supporting documentation needed for your appeal and send it to your insurance company.
How can I find out how my dental insurance claim is progressing?
By getting in touch with your insurance company directly, visiting their website, or using a digital tool or app that your insurer or a third-party service has provided, you can find out the status of your dental insurance claim.
Are there any apps or online resources available to assist with managing dental insurance claims?
Indeed, a variety of digital tools and applications, including those provided by insurance companies, dental offices, and third-party services, are available to assist with managing dental insurance claims. You can stay organized, track claims, and submit paperwork with the aid of these tools.
What are some typical explanations for the denial of dental insurance claims?
Lack of pre-authorization, inaccurate or missing information, non-covered procedures, and exceeding annual maximums are common causes for dental insurance claim denials. You can prevent denials and guarantee a more seamless reimbursement process by being aware of these reasons.
How can I get the most money back for my dental care?
Verify your benefits prior to a procedure, get pre-authorization when necessary, and make sure your dentist provides accurate and comprehensive documentation in order to optimize your dental treatment reimbursement. Know the coverage, deductibles, co-pays, and annual maximums of your insurance plan as well.