It can be difficult to navigate the complicated world of medical billing, particularly when it comes to payment for lab tests. Did you know that every year, millions of dollars in reimbursements are not claimed because people don’t grasp the procedure?
Healthcare providers need a lab test reimbursement guide to make sure they get paid what they are due. Delays and rejections can be greatly decreased by being aware of the forms, deadlines, and online claims procedure.
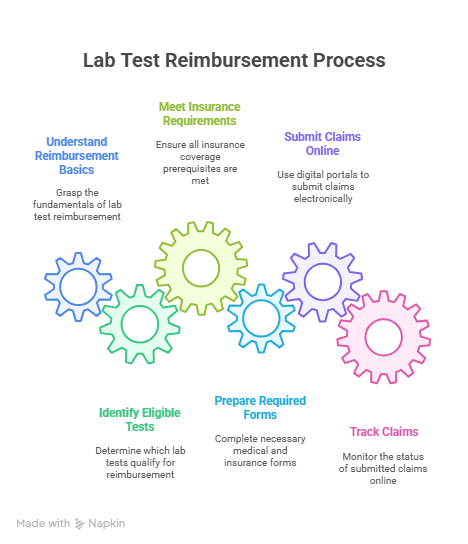
Healthcare providers can concentrate on providing high-quality patient care by streamlining the reimbursement process. We’ll take you through all the necessary steps in this guide so you can easily handle lab test reimbursement.
Understanding Lab Test Reimbursement Basics
For a seamless and effective experience, it is essential to comprehend the fundamentals of lab test reimbursement. The kinds of lab tests that qualify for reimbursement and the prerequisites for insurance coverage are two important aspects of the lab test reimbursement procedure.
Types of Lab Tests Eligible for Reimbursement
Not every laboratory test qualifies for reimbursement. Tests that are considered medically necessary are usually covered. This covers diagnostic procedures like imaging studies, urinalysis, and blood work. To prevent unforeseen costs, it’s critical to know which tests are covered by your plan.
Insurance Coverage Requirements
Lab test coverage under health insurance varies by plan and provider. Lab tests ordered by a healthcare physician and considered medically necessary are typically covered by insurance companies. For some tests, pre-authorization could be necessary. It’s essential to comprehend your insurance coverage in order to guarantee that you get the most money back.
Common Reimbursement Challenges
The reimbursement process for lab tests might present difficulties even with the best of intentions. Frequently encountered problems include erroneous billing, tests that are not considered medically essential, or claims that are denied for lack of pre-authorization. You can handle the process more skillfully if you are aware of these possible obstacles.
Comprehensive Lab Test Reimbursement Guide: Process and Documentation
It is essential to adhere to the proper procedure and provide the necessary paperwork in order to guarantee successful lab test reimbursement. From completing the relevant documents to submitting your claims online, this thorough guide will guide you through every step of the process.
Required Forms and Documentation
Reimbursement for lab tests requires accurate documentation. The following documents and forms are required:
Medical Necessity Forms
To support the lab tests conducted, medical necessity forms must be completed. These forms usually contain a doctor’s signature, test details, and patient information.
Insurance Verification Documents
Usually supplied by the insurance company, insurance verification documents attest to the patient’s coverage.
Proper Coding Requirements
Reimbursement for lab tests depends on accurate coding. This entails describing the lab tests carried out using the appropriate CPT and ICD-10 codes.
Critical Timeframes for Submission
For lab test reimbursement, claims must be submitted on time. It’s crucial to remember the following timelines:
Insurance-Specific Deadlines
Claim submission timeframes vary from a few days to several months, depending on the insurance provider.
Appeals Process Timeframes
The appeals process usually has its own set of deadlines, which can be as short as 30 days, if a claim is rejected.
Follow-up Procedures
Claims must be followed up on in order to guarantee prompt compensation. This may entail getting in touch with the insurance company directly or using the internet to verify the progress of claims.
Online Claims Submission Process
Lab test reimbursement is now more efficient thanks to the online claims submission process. Important elements consist of:
Digital Portals and Platforms
Uploading necessary papers is made simpler by the internet platforms that many insurance companies offer for submitting claims.
Electronic Documentation Tips
Make sure all necessary information is included and that the files are in the right format when submitting electronic documents.
Tracking Your Online Claims
You may effectively follow up by tracking the status of your claims on the majority of online platforms.
Simplifying Lab Test Reimbursement
It might be difficult to navigate lab test reimbursement policies, but knowing how to do it is essential to optimizing your insurance benefits. You can expedite the reimbursement process by becoming familiar with the necessary paperwork, procedures, and deadlines.
Reimbursement rules for lab tests that work assist lower out-of-pocket costs and guarantee that you can afford the medical care you need. Making educated judgments regarding your healthcare is made possible by keeping up with these policies.
You may maximize your insurance coverage and handle lab test reimbursements with confidence by adhering to the rules described in this article.
FAQ
What is the typical timeframe for lab test reimbursement?
Depending on the insurance company and the intricacy of the claim, the turnaround time for lab test reimbursement varies. The average turnaround time for reimbursement is a few days to a few weeks.
What forms are required for lab test reimbursement?
Usually, a claim form, medical necessity forms, and insurance verification documents are needed in order to get compensation for lab tests. Depending on the insurance company and the kind of lab test, several paperwork could be needed.
How do I ensure that my lab test is eligible for reimbursement?
You should confirm that your lab test is covered by your insurance plan and that it is medically required in order to be eligible for payment. Checking your insurance policy or getting in touch with your insurance company directly are two ways to accomplish this.
What is the process for submitting a lab test reimbursement claim online?
Logging onto your insurance provider’s online portal, completing the necessary claim form, and attaching supporting evidence are the usual steps in the online claims submission procedure. After that, you can use the portal to monitor the progress of your claim.
What are some common challenges faced during the lab test reimbursement process?
Denied claims, delayed processing, and unclear communication from the insurance company are typical issues encountered during the lab test reimbursement procedure. It’s critical to thoroughly examine your insurance coverage and contact your insurance provider as necessary in order to overcome these obstacles.
How do I appeal a denied lab test reimbursement claim?
You should get in touch with your insurance company to find out why your lab test reimbursement claim was rejected and to find out more about the appeals procedure. You might have to resubmit your claim or offer more supporting proof.
What are the lab test coding and billing requirements for reimbursement?
Specific codes, such as CPT and ICD-10 codes, must be used to describe the lab test and the diagnosis in order to comply with the billing and lab test coding criteria for payment. For your claim to be processed properly, accurate coding and billing are essential.




