Did you realize that the conventional method of processing medical claims can significantly deplete the resources available to the healthcare system? Manually submitting claims for reimbursement takes a lot of time and is prone to mistakes, which can cause payments to be delayed and administrative burdens to increase.
Online claim submission transforms this procedure by providing a more streamlined, effective, and error-free option. Healthcare providers can greatly lessen the inconvenience of using conventional compensation procedures by utilizing healthcare reimbursement services.
The move to online medical billing reimbursement is revolutionizing healthcare by streamlining and simplifying operations. We’ll go into the details of how online submissions can help healthcare professionals as we continue to examine this subject.
Understanding the Digital Claims Process
The medical billing industry is changing as a result of the move to digital claims processing. The need for efficiency and less administrative work is what is driving this trend. At the front of this change is online revenue cycle management, which helps medical providers better handle claims.
Key Components of Electronic Claim Submission
Medical coding solutions and electronic billing software are two essential elements of electronic claim filing. Together, these resources guarantee that claims are correctly produced and sent to payers. The claims process is streamlined with efficient electronic billing software, which lowers errors and speeds up reimbursement.
Benefits of Paperless Reimbursement Systems
Among the many advantages of paperless reimbursement systems include lower administrative expenses, quicker reimbursement cycles, and more accuracy. Healthcare providers can improve patient happiness and their financial success by implementing online revenue cycle management solutions. One important step toward a more effective healthcare billing process is the move to digital claims processing.
Medical Billing Reimbursement Online: Essential Tools and Software
The transition to online medical billing reimbursement has made the use of sophisticated software solutions necessary. Healthcare providers must use technology that expedites insurance claim processing and complies with telemedicine reimbursement best practices in order to effectively manage the reimbursement process.
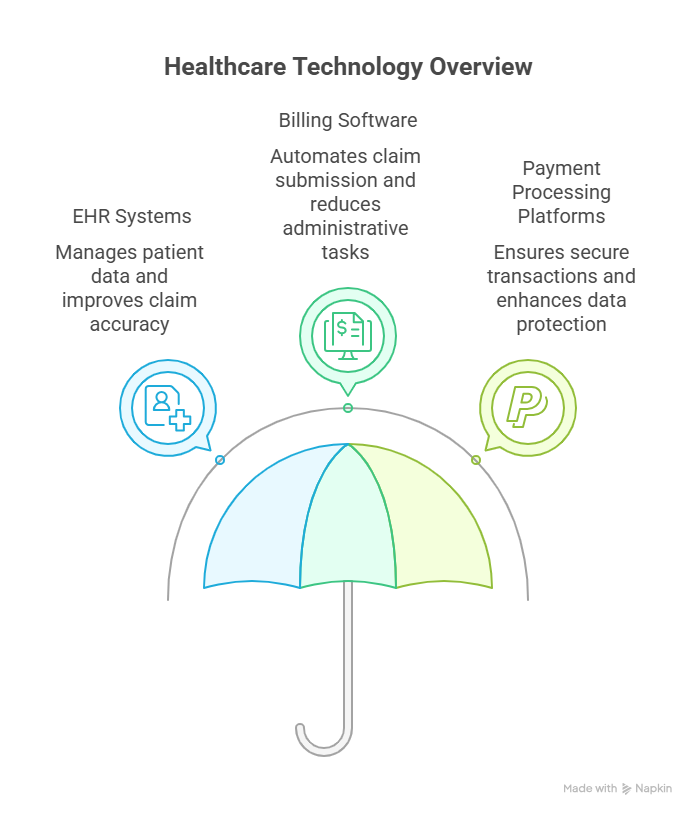
Electronic Health Record (EHR) Integration
For smooth online medical billing reimbursement, EHR integration is essential. It makes it possible for patient data to be transferred accurately and efficiently, which lessens administrative workloads and minimizes mistakes in digital health reimbursement.
Selecting Effective Billing Software Solutions
When choosing billing software, take into account options that include strong features like real-time tracking, automated claim submission, and thorough reporting. These characteristics are necessary for processing insurance claims effectively.
Secure Payment Processing Platforms
Platforms for secure payment processing are essential for safeguarding private patient data while transactions are being conducted. By guaranteeing adherence to legal requirements, these systems protect the patient and the healthcare professional during the telemedicine reimbursement procedure.
| Tool/Software | Function | Benefit |
|---|---|---|
| EHR Systems | Patient data management | Improved accuracy in claim processing |
| Billing Software | Automated claim submission | Reduced administrative burden |
| Payment Processing Platforms | Secure transactions | Enhanced patient data protection |
Step-by-Step Guide to Submitting Claims Electronically
Knowing how to electronically file claims is crucial for navigating the intricacies of online medical billing reimbursement. In addition to expediting the reimbursement period, this procedure lowers the possibility of errors that come with manual submissions.
Preparing Accurate Patient and Insurance Information
Making sure that patient and insurance information is correct and current is the first step in electronically submitting claims. This include confirming policy numbers, insurance coverage information, and patient demographics. To prevent claim denials, accurate data entry is essential.
Proper Medical Coding Practices
For a claim to be submitted successfully, the right medical codes must be used. This entails keeping up with the most recent CPT and ICD-10 codes and making sure the codes are appropriate for the patient’s diagnosis and course of therapy. Appropriate coding procedures promote easier reimbursement and less claim denials.
Submitting and Tracking Claims
After the claim is ready, it can be sent straight to the payer or electronically via a clearinghouse. Monitoring the claim’s progress is crucial for quickly spotting any possible problems. Efficient claim monitoring and reimbursement management can be achieved by utilizing online revenue cycle management systems.
Addressing Common Rejection Reasons
Claims may be denied for a number of reasons, including insufficient data, coding problems, or inaccurate patient information. Typical explanations for rejection include:
- Patient demographics that are inaccurate or lacking
- Inaccurate or inconsistent insurance data
- Outdated or inaccurate medical codes
Healthcare providers should take proactive steps to reduce rejections and guarantee a more seamless medical claims processing experience by being aware of these typical problems.
Conclusion
Adopting digital solutions for online medical billing reimbursement can greatly expedite the claims procedure, lowering stress and increasing effectiveness. Healthcare providers may guarantee correct and timely submissions by utilizing electronic billing software and healthcare reimbursement services.
The digital claims process is further improved by the efficient application of telemedicine reimbursement best practices, which permits smooth connection with current systems. Adopting digital reimbursement solutions is essential to remain ahead of the curve as the healthcare sector continues to change.
Healthcare providers can lower expenses, increase patient happiness, and eliminate errors by putting these digital solutions into practice. Online medical billing reimbursement thus turns into a useful tool for providing patients with top-notch service.
FAQ
What is medical billing reimbursement online?
The practice of electronically submitting medical claims to insurance companies for payment is known as “online medical billing reimbursement.” The reimbursement procedure is streamlined by this digital method, which also increases efficiency and decreases paperwork.
How does electronic claim submission work?
Medical claims are prepared and submitted to insurance companies electronically using specialist software. To guarantee correct and timely claim submission, this procedure usually entails integrating with practice management systems and Electronic Health Records (EHRs).
What are the benefits of using online revenue cycle management for medical billing?
The medical billing process can be streamlined with the aid of online revenue cycle management, which can improve cash flow and lessen administrative workloads. Additionally, it can assist in recognizing and resolving typical problems that result in claim denials.
How can I ensure accurate medical coding for claim submission?
For a claim to be submitted successfully, accurate medical coding is essential. Accuracy can be ensured by using current medical coding systems and keeping up with code changes. Errors can also be reduced by collaborating with knowledgeable code experts.
What are some best practices for telemedicine reimbursement?
Healthcare providers should confirm patient insurance coverage, follow proper coding and billing procedures, and keep thorough records of telemedicine services in order to guarantee effective telemedicine reimbursement. It’s also critical to keep up with evolving rules and regulations.
How can I track the status of my submitted claims?
You can trace the progress of your filed claims with the help of claim tracking tools found in many electronic billing software packages. To find out the status of your claim, you can usually get in touch with your insurance company directly.
What are some common reasons for claim rejections, and how can I avoid them?
Inaccurate patient or insurance information, coding mistakes, and missing or insufficient paperwork are frequent causes of claim denials. Make sure that data entry is correct, keep up of coding modifications, and carefully examine claims before to submission in order to prevent these problems.
How can I ensure secure payment processing for medical billing reimbursement?
Healthcare providers should collaborate with trustworthy payment processing systems that adhere to pertinent security standards, such PCI-DSS, to guarantee secure payment processing. Sensitive patient data can also be protected by putting strong security measures in place, such as access limitations and encryption.