With billions of dollars in revenue on the line, the healthcare sector is a complicated and dynamic landscape. It is astounding to learn that healthcare providers lose an estimated $68 billion in income each year as a result of inaccurate coding and billing errors. This emphasizes how crucial it is to comprehend reimbursement policies in order to optimize financial well-being.
For healthcare practitioners to successfully navigate this complex system, a thorough medical coding reimbursement guide is necessary. Providers can streamline their revenue cycle and guarantee regulatory compliance by understanding the basics of reimbursement. We will explore the realm of medical code reimbursement in this post, giving readers a comprehensive grasp of the essential components and insights into comprehending reimbursement policies.
Understanding the Medical Coding Reimbursement Guide
Navigating the complex world of medical coding reimbursement requires a deep understanding of the underlying systems and processes. To effectively manage reimbursement, healthcare providers must be well-versed in the basics of medical coding systems, how reimbursement works in healthcare, and the latest updates in coding reimbursement guidelines.
The Basics of Medical Coding Systems
The foundation of the reimbursement procedure is medical coding systems. These systems, like CPT and ICD-10, offer a consistent method for categorizing operations and diseases. For healthcare providers to be properly compensated for their services, accurate coding is essential.
For instance, diagnoses are categorized using the ICD-10 system, which is updated yearly to account for advancements in technology and medical procedures. To maximize their reimbursement procedures, healthcare practitioners must comprehend the subtleties of these coding schemes.
How Reimbursement Works in Healthcare
Reimbursement in healthcare involves a complex interplay between healthcare providers, insurance companies, and government programs. The process begins with the healthcare provider assigning the appropriate codes to the patient’s diagnosis and treatment using medical coding systems.
Insurance companies and government programs then use these codes to determine the level of reimbursement. The reimbursement process can be influenced by various factors, including the type of insurance coverage, the patient’s condition, and the treatment provided.
Recent Updates in Coding Reimbursement Guidelines
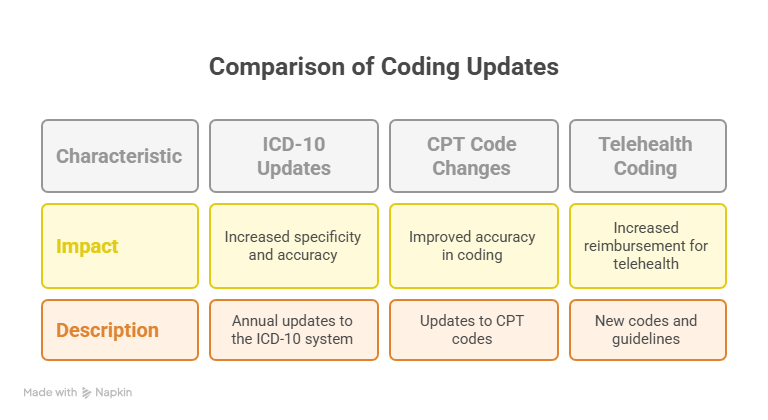
Guidelines for coding reimbursement are always changing to take into account modifications to healthcare legislation, technology, and medical procedures. In addition to addressing new concerns including value-based care and telemedicine, recent upgrades have concentrated on increasing the precision and specificity of coding.
Healthcare providers must keep abreast of these developments in order to guarantee compliance and optimize payment. Some of the most significant recent changes to the coding reimbursement criteria are compiled in the table below:
| Update | Description | Impact |
|---|---|---|
| ICD-10 Updates | Annual updates to the ICD-10 system to reflect changes in medical practices and technology. | Increased specificity and accuracy in coding diagnoses. |
| CPT Code Changes | Updates to CPT codes to reflect changes in medical procedures and services. | Improved accuracy in coding procedures and services. |
| Telehealth Coding | New codes and guidelines for telehealth services. | Increased reimbursement for telehealth services. |
Healthcare providers can streamline their reimbursement procedures and guarantee they are fairly compensated for their services by being aware of the fundamentals of medical coding systems, how healthcare reimbursement operates, and the most recent revisions to coding reimbursement criteria.
Strategies for Maximizing Medical Coding Reimbursement
The financial performance of a healthcare provider can be significantly impacted by comprehending and putting into practice the appropriate medical code reimbursement procedures. A multifaceted strategy that include precise coding, effective workflows, and technology use is needed to maximize medical coding reimbursement.
Best Practices for Accurate Coding
Successful medical coding reimbursement is based on accurate coding. Healthcare practitioners must keep abreast of the most recent coding standards and rules in order to accomplish this. Among the finest practices are:
- Frequent Training: Make certain that coding personnel are regularly instructed on new rules, guidelines, and codes.
- Coding Audits: To find and fix coding mistakes, do routine audits.
- Use of Coding Resources: To stay up to date, make use of trustworthy coding resources, such as the CPT codebook published by the American Medical Association.
Avoiding Common Reimbursement Pitfalls
Reimbursement requests may be rejected for a number of reasons, even with the best efforts. Typical pitfalls consist of:
- Inaccurate Patient Information: Ensure that patient demographic information is accurate and up-to-date.
- Insufficient Documentation: Provide thorough documentation to support the codes used.
- Non-Compliance with Payer Policies: Stay informed about payer policies and comply with their requirements.
Implementing Efficient Reimbursement Workflows
In order to maximize reimbursement, efficient workflows are essential. This can be accomplished by:
Documentation Improvement Tips
Reducing refused claims requires better documentation. Some pointers are:
- Clear and Concise Documentation: Make certain that all documentation is easily readable, clear, and concise.
- Timely Documentation: To prevent delays, record patient information as soon as possible.
Technology Solutions for Better Reimbursement
Utilizing technology can greatly improve the reimbursement procedure. Among the solutions are:
- Electronic Health Records (EHRs): Utilize EHRs to streamline documentation and coding processes.
- Reimbursement Software: Implement software designed to optimize reimbursement by identifying potential issues before claims are submitted.
Conclusion
Reimbursement for medical codes is a complicated but essential component of healthcare administration. Healthcare providers can maximize reimbursement and guarantee financial stability by understanding the basics of medical coding systems and keeping abreast of payment regulations.
Navigating the complexities of healthcare payment requires a thorough comprehension of the medical coding reimbursement guide. In order to maximize reimbursement potential, this entails putting best practices for precise coding and effective workflows into practice.
It’s critical for healthcare professionals to stay knowledgeable and flexible as the industry changes. Healthcare workers can successfully negotiate the opportunities and difficulties in medical code reimbursement by utilizing the knowledge and tactics offered in this guide, guaranteeing a secure financial future.
Maintaining current knowledge of reimbursement criteria can help healthcare professionals make wise choices and succeed in a constantly evolving healthcare landscape.
FAQ
What is medical coding reimbursement, and why is it important?
The process by which healthcare practitioners get compensated for their services using the codes linked to diagnoses and procedures is known as medical coding reimbursement. It is vital for optimizing income and guaranteeing adherence to regulatory requirements since it has a direct impact on the financial stability of healthcare providers.
How do medical coding systems impact reimbursement?
Diagnoses and procedures are categorized using medical coding systems like ICD-10 and CPT, which are then used to calculate reimbursement rates. For healthcare providers to be fairly compensated for their services, accurate coding is essential.
What are some common reimbursement pitfalls, and how can they be avoided?
Coding mistakes, inadequate documentation, and a failure to keep abreast of evolving regulations are common reimbursement pitfalls. Healthcare providers should use accurate coding best practices, enhance documentation, and keep up with changes to coding reimbursement guidelines in order to avoid these pitfalls.
How can technology solutions enhance medical coding reimbursement?
Automated coding software and electronic health records (EHRs) are two examples of technological solutions that can increase efficiency, decrease errors, and streamline reimbursement procedures. Healthcare providers can increase revenue and streamline their reimbursement processes by utilizing these solutions.
What are some strategies for maximizing medical coding reimbursement?
Maintaining current knowledge of coding guidelines, putting in place effective reimbursement workflows, and enhancing documentation are some tactics for optimizing medical coding reimbursement. To guarantee adherence to evolving regulations, healthcare providers should also periodically assess and update their coding procedures.
How often do coding reimbursement guidelines change, and how can healthcare providers stay informed?
Coding reimbursement guidelines are subject to frequent changes, usually taking place on an annual or quarterly basis. Attending industry conferences or workshops and routinely reviewing updates from pertinent authorities, like the Centers for Medicare and Medicaid Services (CMS), are two ways healthcare providers can stay informed.
What role do insurance companies and government programs play in medical coding reimbursement?
Insurance companies and government programs, such as Medicare and Medicaid, play a significant role in medical coding reimbursement by determining reimbursement rates and setting guidelines for coding and billing. Healthcare providers must understand the specific requirements and regulations of each payer to ensure accurate reimbursement.




