Did you know that a lack of knowledge about insurance coverage details results in almost 30% of prescription medication costs going unpaid? For many people, this can result in large out-of-pocket costs.
Comprehending insurance coverage for pharmacy reimbursement is essential for controlling medical expenses. It entails being aware of which drugs are covered, how to submit claims, and what paperwork is needed.
Understanding the fundamentals of pharmacy insurance reimbursement can help people drastically lower their medical costs. This post will walk you through the steps, outlining what is covered and how to submit a reimbursement application.
Understanding Pharmacy Reimbursement Insurance Coverage
It’s critical to comprehend your pharmacy insurance coverage in order to control medical expenses.The amount that your insurance company will pay for your prescription drug costs depends on your pharmacy reimbursement insurance coverage.
Common Types of Pharmacy Insurance Plans
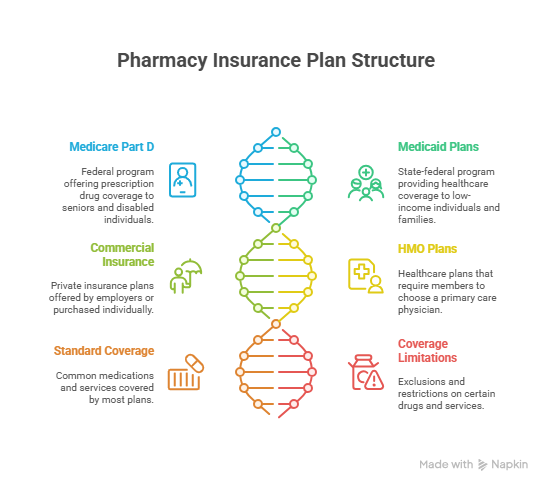
Pharmacy insurance plans come in a variety of forms, such as:
- Plans under Medicare Part D
- Plans for Medicaid
- Plans for commercial insurance
- Plans from Health Maintenance Organizations (HMOs)
Every plan has a unique list of services and drugs that are covered.
Standard Covered Medications and Services
A variety of drugs and services are covered by the majority of pharmacy insurance plans, including:
- Prescription drugs
- Generic drugs
- A few over-the-counter (OTC) drugs
Making educated healthcare decisions can be facilitated by being aware of what your plan covers.
Coverage Limitations and Exclusions
Understanding your pharmacy insurance plan’s exclusions and limitations is crucial. Certain drugs or services might not be covered by some plans, including:
- Treatments that are experimental
- Some name-brand drugs
You can learn more about what is and is not covered by going over the documentation for your plan.
The Pharmacy Reimbursement Process Explained
Making the most of your insurance coverage can be achieved by understanding how pharmacy reimbursement operates, which is an essential component of healthcare. Benefit management systems, pharmacies, and insurance companies are among the many parties involved in the process.
How Insurance Companies Determine Reimbursement Rates
The type of medication, the pharmacy’s network status, and the patient’s coverage plan are some of the variables that insurance companies consider when determining reimbursement rates.Reimbursement amounts are largely determined by the rates that insurance companies and pharmacies negotiate.
Pharmacy Benefit Management Systems
Systems for Pharmacy Benefit Management (PBM) are essential for controlling pharmacy reimbursement. PBMs serve as a bridge between patients, pharmacies, and insurance companies, expediting the reimbursement procedure and guaranteeing effective claim processing.
How to Apply for Pharmacy Insurance Reimbursement
Pharmacy insurance reimbursement applications can be intimidating, but they are simple to complete with the correct help.
Required Documentation for Claims
You will need to collect certain documents in order to start the reimbursement process. These usually consist of a filled-out claim form, prescription receipts, and your insurance ID. To prevent delays, it is essential to make sure that all documents are correct and comprehensive.
Step-by-Step Application Process
Several crucial steps are involved in the application process:
- Gather all required paperwork.
- Complete the claim form completely.
- Use the appropriate method to submit the claim (online, by mail, or in person).
- Monitor the status of your claim.
Common Reasons for Claim Denials
Claims may be rejected for a number of reasons, such as:
- information that is erroneous or incomplete.
- services or drugs that are not covered.
- missing records.
You can steer clear of these typical pitfalls by being aware of them.
Tips for Appealing Denied Claims
Don’t be afraid to appeal if your claim is rejected. Make sure you comprehend the rationale behind the rejection, obtain more supporting evidence if required, and make a succinct, understandable appeal.
| Documentation | Purpose | Tips for Submission |
|---|---|---|
| Insurance ID | Verifies insurance coverage | Ensure it’s legible and up-to-date |
| Prescription Receipts | Proves purchase of prescribed medication | Keep all receipts, including those for copays |
| Claim Form | Officially submits claim for reimbursement | Fill out completely and accurately |
Maximizing Your Pharmacy Insurance Benefits
Making the most of your pharmacy insurance benefits requires an understanding of your pharmacy reimbursement insurance coverage. You can reduce the cost of your prescription drugs and medical services by being aware of what is covered and how to submit an application for reimbursement.
It’s crucial to become familiar with the pharmacy reimbursement procedure, including the necessary paperwork and the detailed application process, in order to optimize your benefits. You can also steer clear of potential pitfalls by being aware of the typical explanations for claim denials.
You can confidently navigate the pharmacy reimbursement insurance coverage and make sure you get the benefits to which you are entitled by using the information you have learned from this article. Make the most of your pharmacy insurance benefits and keep yourself informed.
FAQ
What is pharmacy insurance reimbursement?
The process by which insurance companies reimburse pharmacies for the drugs and services they provide to their policyholders is known as pharmacy insurance reimbursement.
How do I know if my medication is covered under my pharmacy insurance plan?
To find out if your prescription is covered, visit the website of your insurance company or get in touch with customer support. You can also speak with your pharmacist or go over the details of your insurance policy.
What is the difference between a pharmacy insurance plan and a pharmacy benefit management system?
A pharmacy benefit management system is a third-party administrator that oversees pharmacy benefits on behalf of insurance companies, whereas a pharmacy insurance plan is a form of insurance coverage that aids in the payment of prescription drugs.
How are pharmacy reimbursement rates determined?
Insurance companies usually base pharmacy reimbursement rates on a number of factors, including dispensing fees, the average wholesale price of a medication, and other expenses.
What are some common reasons for pharmacy insurance claim denials?
Lack of prior authorization, inaccurate or missing claims information, and prescription drugs not covered by the insurance plan are common causes of claim denials.
How can I appeal a denied pharmacy insurance claim?
In order to challenge a denied claim, you can get in touch with your insurance company to find out why it was rejected and to submit more supporting documentation or information. You can also file an appeal or resubmit the claim in collaboration with your pharmacist.
What documentation is required for pharmacy insurance reimbursement claims?
A valid prescription, evidence of insurance coverage, and a filled-out claim form are usually required documents. Depending on the particular insurance plan and claim type, more paperwork might be needed.
Can I use my pharmacy insurance coverage at any pharmacy?
The network of your insurance plan determines this. You can get discounted prices at a network of participating pharmacies that are part of many insurance plans. Employing an out-of-network pharmacy could lead to increased expenses or claims being rejected.




